Medical professionals, say doctors Arun Gadre and Abhay Shukla, should be saving lives, not depleting life savings. In a new book, they expose the malaise of Indian health care

Dr Abhay Shukla and Dr Arun Gadre
When a teenager’s family approached me for a second opinion about terminating an unwanted pregnancy, I discovered that the girl was not pregnant to begin with. The family was shown someone else’s blood work to convince them of the need for an abortion," says Pune-based gynaecologist, Dr Arun Gadre.
ADVERTISEMENT
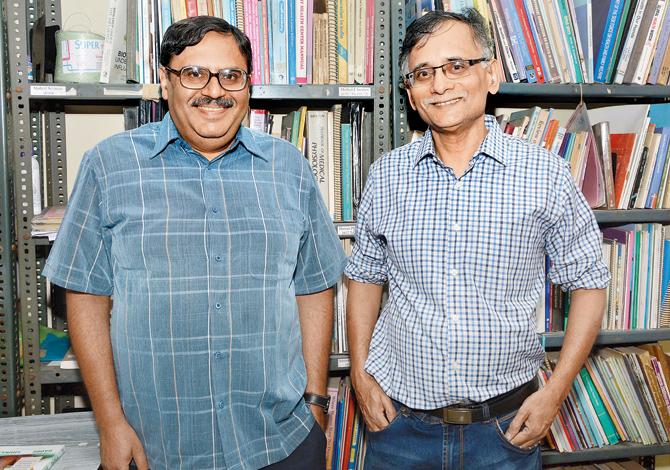
Dr Abhay Shukla and Dr Arun Gadre. Pic/Vaishali Galim
Stories like these pack the pages of Penguin-Random House India title, Dissenting Diagnosis, which Gadre has co-authored with Dr Abhay Shukla, a public health physician. With testimonials from 78 doctors practicing in six states and across 23 fields of medicine (including traditional), the book spares no one. From big "hospital malls" right down to autorickshaw drivers (paid to direct patients to specific clinic), it claims, everyone is on the take.
Speaking about the challenges of embarking on a crusade against their mother-ship, Shukla says, "Medicine, is like a guild — we’re like craftsmen, an intermediate category between say, scientists and artists. There’s a code of honour among doctors and while they may compete, publicly, one doctor will not criticise another."
Meanwhile, health care bills drive 3.5 crore Indians into poverty each year, write the doctors who propose a list of reforms in the second half of their title. One item on their list is an efficient regulatory body. Extoling the government’s 92nd report on the Medical Council of India, Shukla explains, "Regulatory bodies that exist today are inward-looking, closed committees, incestuous groups that lack openness and hence fail to check their own members. Their panels have no civil society representatives, no health activists or representatives from patients’ rights groups. Consequently, they’re un-critical about themselves, and there’s a large number of pending complaints with no machinery to deal with these. In Maharashtra, for example, there’s an ethics committee (comprised of doctors who volunteer) that meets once a week. It has no dedicated investigative wing that looks into complaints."
At the same time there’s the problem of too many centres of governance and unethical practices slip between the loopholes in the confusion, adds Dr Gadre. "With regard to the transgressions of trust hospitals, for instance, many of which flout their responsibility of reserving 10 per cent of beds for indigent patients (entitled to free treatment) and another 10 per cent for economically weaker sections of society (entitled to heavily subsidised treatment), it is the charity commissioner who is responsible to take action. The medical council would say this is not our lookout."
Translated in part from Gadre’s report which was originally in Marathi, where the book disappoints is in the style and flow of narrative. A more powerful statement may have been made by getting first-person accounts from patients rather than having the fraternity describe unscrupulous practices of un-named colleagues.
The book also seems tinted with a deep shade of socialism. Surely, it’s unfair to deny an especially skilled surgeon a premium for her service. Gadre takes a different view. "Here in India, we tend to worship people — he has a good hand, etc. — this is wrong. I assure you that any person who has gone through a good teaching regime and proper exams is equally skilled." He explains why free market mechanics cannot apply. "Here, consumer is not king. The doctor-patient relationship is hinged on trust and there is an imbalance of knowledge. When you buy soap, you're free to pick any brand you like, but the
doctor is entrusted with the job of thinking on behalf of the patient."
Aside from a fixed tariff for treatments (subject to a very limited variation based on the quality of the facility and/or complications in the procedure), the doctors advocate strictly against private medical colleges that charge exorbitant fees, saying their graduates then do all they can to recover these from patients. Shukla says the question to ask is what kind of doctors do we need. "We need doctors who are drawn socially…who are willing and committed to provide service where it is genuinely required."
Recommending the sort of three-year medical courses introduced in Venezuela and Cuba, Shukla says a 10-year bond should be introduced to compel graduating doctors to work in rural areas.
He admits that a two-year stipulation does already exist in some states like Maharashtra. "But, as it stands, the medical education department is responsible for enforcing the bond and the public health department then has to place the doctors. So, if they make doctors available on paper and the public health department does not place them, it amounts to nothing. Besides, in their rush to enter lucrative private practices, many pay the bond amount of R10 lakh and skip the rural stint. We must make it compulsory, like it is in Thailand. The skills gained by working in a district hospital or a crowded public hospital are invaluable. Most of those who graduate from private medical colleges can do little more than prescribe ultrasounds
and lab tests."
 Subscribe today by clicking the link and stay updated with the latest news!" Click here!
Subscribe today by clicking the link and stay updated with the latest news!" Click here!