While a majority of neurosurgeons and psychiatrists seek more research before surgery is considered to treat psychiatric disorders, a few doctors are taking the chance, albeit with caution

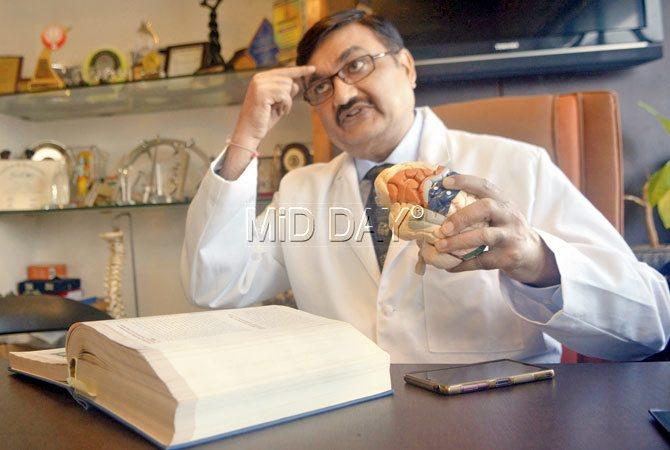
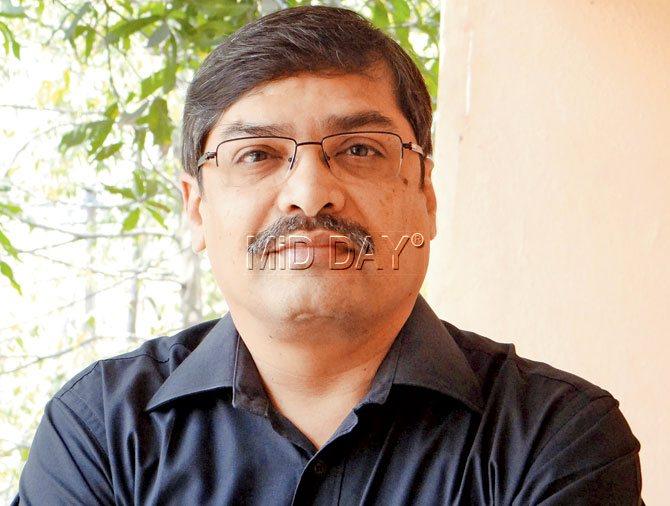
Dr Sanjay Mongia and Dr Paresh K Doshi are among the few Indian practitioners of functional neurosurgery for OCD and depression. Pics/Shadab Khan and Pradeep Dhivar
Benjamin Ward mails us a selfie. It’s of him with fiancé Alyssa, both flashing wide smiles. It’s a precious picture, not just because the two are to marry next January, but also for Ward’s expression.

(Above) Dr Sanjay Mongia and Dr Paresh K Doshi (below)are among the few Indian practitioners of functional neurosurgery for OCD and depression. Pics/Shadab Khan and Pradeep Dhivar

This is a man who claims he had forgotten to smile for five years while battling treatment resistant depression in Sydney where he worked as a professional carpenter. His parents, Lyndal and Colin Ward were habituated to seeing him return home early from work, sometimes sobbing uncontrollably.
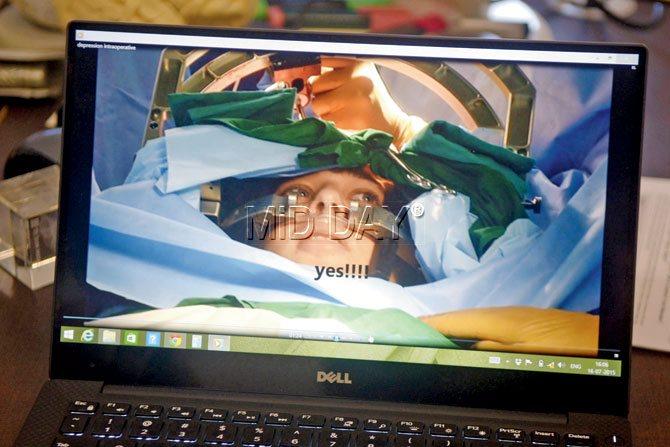
A video of Australian patient Benjamin Ward’s surgery done in 2013, shows Dr Doshi asking him at each placement of the electrode if he is feeling better. “You have to find the sweet spot,” Dr Doshi says of the procedure
“I was unable to work or meet people. Often, I’d contemplate suicide,” says Ward, 28, over the phone from Sydney. Between 2008 and 2013, he tried 15 varieties of anti-depressants. Electroconvulsive Therapy (ECT), a technique that attaches electrodes on a patient’s scalp to allow a finely controlled electric current to reach him under general anesthesia, offered relief that barely lasted weeks.

Australian Benjamin Ward, 28, with fiance Alyssa. Before Ward was operated using DBS in Mumbai, he suffered from treatment resistant depression for five years
His incessant research led him to Deep Brain Stimulation (DBS) surgery. It requires that two 1.1 mm wires are inserted into the patient’s brain, and connected to a pacemaker placed under the skin of the chest. Providing a continuous stream of electricity, it stimulates the affected part of the brain, which in the case of depression, is the sub-genu cingulate gyrus. This helps relieve depression, say experts of functional neurosurgery. PET scan studies have revealed that previously hypo functioning areas of depression became hyper functioning post-treatment, confirming that the condition was reversible.
Ward was led to Mumbai-based stereotactic and functional neurosurgeon at Jaslok Hospital & Research Centre, Dr Paresh K Doshi. In October 2013, Ward underwent a five-hour surgery to cure him of unflagging sadness.
DBS can be reversed. “If the electrode isn’t working, you can remove it,” says Dr Doshi
The inner circle
Sitting in his cabin on the 11th floor of the Peddar Road hospital, Doshi says he grew interested in functional neurosurgery, a stream concerned with altering and correcting the central nervous system’s (brain and spinal cord) physiology or normal function, as a medical student at Nair Hospital. Within a year of his return from London’s National Hospital for Neurology and Neurosurgery, he joined Jaslok. In 1998, he was off to France to train in DBS, a procedure used on Ward and one that has been commonly used worldwide to treat patients suffering from Parksinon’s, since the late 1990s. Its use in epilepsy was recognised in 2008.

Dr Samir Parikh, Fortis Healthcare
For the last five years, however, functional neurosurgery is also being used to treat psychiatric disorders, including depression, and more commonly, obsessive compulsive disorder (OCD).

Dr Sanjay Mongia, Asian Heart Institute
“In 2010, while going through some world literature in the field, I realised that it was possible to use DBS for certain psychiatric ailments, too. After much research and setting up ethical guidelines at our hospital, we decided to offer it to psychiatric patients,” says the 52-year-old.
This makes Doshi one among just a handful of doctors in the country who use popular neurosurgical procedures, amidst much debate, to treat depression and OCD.
He walks up to his shelf to bring out a volume of Textbook of Sterotactic and Functional Neurosurgery by Andres M Lozano, Philip L Gildenberg and Ronald R Tasker. Recounting the history of psycho surgery, he speaks of American physician Walter Freeman and neurosurgeon James Watz, who in the 1940s, became advocates of lobotomy. The highly controversial procedure required them to severe connections to the prefrontal cortex in the frontal lobes of the brain. “Freeman and Watz,” says Doshi, “went berserk.
They’d travel across the US in a van with an ice pick, cutting the sub frontal fibres of patients who were brought to them. Between 1935 and 1950, it is estimated that 90,000 such procedures were conducted across the world,” he shares. Patients were ‘treated’ for depression, schizophrenia, aggression and other mental health disorders. However, because their limbic system — the primary house for the brain’s emotional responses — was cut off, patients would turn apathetic and lethargic. In the 1960s, there was a turnaround in psychiatric care when it was discovered that administering a specific dose of drug chloropromazine would help treat patients with serious schizophrenia, and surgery wasn’t the only option. Now, there are anti-depressants (used on depression and OCD patients), mood stabilizers (for bipolar disorder) and anxiolatics (for anxiety disorders) in the market.
Screening the patient
However, as Ward will tell you, not all patients respond to drugs and Cognitive Behaviour Therapy as well as others.
Which is why doctors like Doshi ensure that the patients they take on are chronic resistant cases.
“We only take on patients referred by a psychiatrist,” says Dr Sanjay Mongia, 45, Mumbai-based neurosurgeon, who uses the Gamma Knife procedure to operate on patients suffering from OCD. “They should have taken medication for at least seven years, and undergone 10 to 20 therapies from multiple psychologists without much relief, for me to consider them for surgery,” he says when we meet him at the Asian Heart Institute, Bandra Kurla Complex.
Dr Y C Janardhan Reddy, NIMHANS
The three-hour-long Gamma Knife procedure is a non-invasive method in which tiny beams of radiation are focused on a specific spot of the brain to create lesions in affected parts. “A patient suffering a mental health condition experiences neuro-chemical changes in the brain. These in turn lead to neuro-physiological changes. When we conduct surgery, we target a particular area of the brain, and create lesions (or damage specific cells) that affect those nuclei or group of cells that are causing the chemical imbalance in the first place,” he explains.

Dr Mohit Bhatt, Kokilaben Dhirubhai Ambani Hospital
In the five years that Mongia has been using Gamma Knife for OCD (all his surgeries have been conducted on patients outside Mumbai), he has treated a total of 20 patients. “I have rejected at least twice the number,” he says.
Doshi, too has performed DBS for depression on Ward and used ablative surgery (creating lesions in the brain by using a radio-frequency electric generator which transfers the electrical current into heat at the tip of the electrode, producing a thermal lesion immediately) on just three others suffering from psychiatric disorders; two of them with OCD and a third with OCD and depression.
A major problem, Doshi believes, is that most patients, especially Indians, don’t maintain a detailed drug history. “We need to know the line of treatment that a patient has received in the five to 10 years before they came to us. Which drugs, what dosage and duration of intake are all crucial information.” Even if a patient is referred to him, he will ask them to first consult Jaslok’s in-house psychiatrist, Dr Amit Desai and neuro psychologist Dr Shraddha Shah, to ensure that the patient is indeed a case fit for surgery.

Which is why a medical student from north Maharashtra, who approached Doshi, was first asked to consult a Thane psychologist for Cognitive Behaviour Therapy.
Time for success
“I have been suffering from OCD for 15 years,” says the 25-year-old over the phone. “I constantly clean my book covers, or adjust the car mirror. I can’t stop. I seek perfection in everything. Even a dog ear in a book will keep niggling me,” he says. The problem has affected his studies, making him repeat the second year of MBBS. While his family, he says, is aware of his condition, his friends haven’t been told yet. “I found out about Dr Doshi and arrived in Mumbai last week to consult him,” he adds.
Yet, it’s patients who are enthusiastic about a surgical solution who need the sternest warning. Besides, results are slow to show. While Ward says it took him two months post-surgery to “become completely okay”, most doctors advise a wait-and-watch period of at least a few years, where the post-operative treatment will include medication and therapy. “This is not an appendectomy where on removing the offending organ, everything will be fine,” says Dr Y C Janardhan Reddy, professor of psychiatry and consultant, Obsessive-Compulsive Disorder Clinic at the Department of Psychiatry in National Institute of Mental Health & Neurosciences (NIMHANS), Bengaluru.
Two years ago, NIMHANS started using the Gamma Knife procedure, to treat patients with severe OCD. It was an extension of their clinical service. Of these, they have seen good results with only one. The statistics, he says, are neither encouraging nor discouraging. “This is science; you are not going to see miracles. We will have to treat 20 to 25 patients to acquire a statistic. You can’t abandon a practice based on three cases,” he points out. The success rates, most say, range between 60 to 70 per cent. After all, even if the electrodes are attached to the right spot, accurate strength of current administered and lesions created, a hundred other factors can vary.
While DBS comes with the attraction of reversibility — “if the electrode isn’t working, you can remove it,” says Doshi — and the Gamma Knife will leave you with transient headaches and dizziness (its most common side effect), the challenge, says Mongia, is also that MRIs and PET Scans that have helped identify the region of the brain where depression or OCD sits, can’t identify the exact spot. This is why, a DBS is done while the patient is awake. For instance, in a video of Ward’s surgery, Doshi is seen asking him at each placement of the electrode if he is feeling better. “You have to find the sweet spot,” he says.
This is also why, though research has shown that regions that control OCD could also control alcoholism, it isn’t specific and established yet. And though, it is believed that psychosurgery may help relieve bipolarism and schizophrenia, much more research needs to be done.
And then, the caution
Dr Mohit Bhatt, in fact, believes far too little research has been done into the subject. Director for Neurosurgery at Andheri’s Kokilaben Dhirubai Ambani Hospital and Research Centre, he says, “My main reservation is that a patient with Parkinson’s has a simple presentation, and the area in the brain where the problem exists can be delineated. You can put an electrode there and correct it. This has been proved in thousands of surgeries and animal experiments. However, no such model exists for psychiatric problems.”
He argues that there is no crisp border of abnormal area for psychiatric disorders. Additionally, psychiatric problems are difficult to assess. “It’s not just physical, but emotional, behavioural presentations too. And these differ in socio-economic groups. The emotional reaction of a depressed person in India will not be the same as that from another part of the world. Also, how a person feels fluctuates every day. We need a good scientific model first.”
Dr Samir Parikh, Director of Mental Health and Behavioral Sciences at Fortis Healthcare, believes surgery should be the last resort. “In the last five years, I would have considered surgery for, say, two patients, but I didn’t end up referring them. The percentage of people who will not respond to any line of treatment is miniscule,” he says, adding that with more awareness on mental health issues, people will consult doctors in the early stages, making psychosurgery even less essential.
For now, however, Ward is glad the option was available to him. “I am back at work full-time and able to do all that I enjoy,” he laughs. “I am riding my motorbike, meeting friends and going to the beach.”
 Subscribe today by clicking the link and stay updated with the latest news!" Click here!
Subscribe today by clicking the link and stay updated with the latest news!" Click here!